Description
Latin name
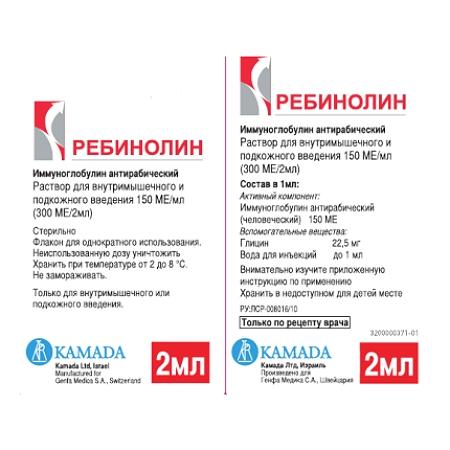
Rebinolin
Form
release solution for injections
Packing
Bottle 2 ml.
Pharmacological action of
Rebinolin is an isotonic buffered solution of a specific human anti-rabies immunoglobulin obtained from donor plasma immunized with an inactivated rabies prophylaxis vaccine (prepared from a strain grown on a human diploid cell culture) and containing a large number of specific antibodies against the virus . Administration immediately after infection forms a passive immunity to rabies virus, increases the incubation period, and this contributes to effective vaccination during complex rabies immunoprophylaxis.
Indications
Treatment-and-prophylactic rabies immunization against any damage to the skin (bites, any wounds and scratches) caused by wild or domestic animals, sick with rabies, with suspected rabies, under veterinary observation and outside of it, as well as during on the mucous membranes or damaged skin of the saliva of infected animals.
Contraindications
Does not exist (100% mortality with rabies overrides any contraindications).
Caution: in patients with documented allergies to any component of the drug.
Use during pregnancy and lactation
The use of this drug during pregnancy has not been studied in controlled clinical trials, therefore, during pregnancy and lactation, the drug should be prescribed only in cases where the expected benefit of therapy for the mother outweighs the potential risk to the fetus or infant. Long experience in the medical use of immunoglobulins does not allow us to expect any harmful effects on the course of pregnancy, as well as on the fetus and newborn.
It should be borne in mind that immunoglobulins are excreted in breast milk, which may facilitate the transfer of protective antibodies (passive immunity) to the baby.
Composition
1 ml contains:
active substance: anti-rabies immunoglobulin 150 IU
Dosage and administration
Intramuscularly, for adults and children – 20 IU / kg (0.133 ml / kg), once. The dose should not be exceeded under any circumstances, as administration of immunoglobulin can partially suppress the production of own antibodies. If the introduction is anatomically possible, the maximum allowable part of the dose should be administered by infiltration around the wound, and the remainder should be administered intramuscularly (in the upper outer quadrant of the buttock). Avoid the central part of the gluteal region, as there is a risk of damage to the sciatic nerve.
At the same time, the first dose of the rabies prophylaxis vaccine (prepared on the culture of human diploid cells) is introduced into another part of the body, preferably as far as possible from the injection site of the anti-rabies immunoglobulin (preferably into the deltoid region).
If therapy was delayed for any reason, the drug should be administered no later than the eighth day after the first dose of the vaccine, regardless of the time interval between exposure to the virus and the start of therapy.
The drug cannot be administered using the same syringe or in the same anatomical area of the body as the rabies vaccine.
To ensure good infiltration of affected areas of the body in children (especially those with multiple injuries), the dose of the drug can be diluted 2-3 times in 0.9% sodium chloride solution.
An anti-rabies immunoglobulin should be administered exclusively in combination with a rabies vaccine. The only exception is persons that have already been vaccinated with a rabies vaccination and that have confirmed the presence of rabies antibodies. These individuals should receive only the vaccine.
Therapy should be discontinued if the animal remains healthy for a 10-day observation period or if the rabies virus is not found in the sacrificed animal after appropriate laboratory testing.
Side effects
Local reactions: soreness and discomfort at the injection site.
Systemic reactions: hyperthermia, allergic reactions (skin reactions, anaphylactic shock, angioedema), dizziness, vomiting, decreased blood pressure, tachycardia.
Drug Interaction
Increases toxicity of cardiac glycosides (due to hypokalemia due to increased risk of arrhythmias). Accelerates the removal of ASA, Reduces the effect of hypoglycemic drugs increases the anticoagulant effect of coumarin derivatives. Reduces the effect of Vitamin D on Ca2 + absorption in the intestinal lumen. Ergocalciferol and parathyroid hormone interfere with the development of osteopathy caused by ACS. Reduces the concentration of praziquantel in the blood. Ketoconazole reduces the clearance and increases the toxicity of methylprednisolone. Co-administration with ciclosporin causes mutual inhibition of metabolism – the risk of side effects of both drugs (with joint use, cases of seizures have been noted). Thiazide diuretics, carbonic anhydrase inhibitors, other ACS and amphotericin B increase the risk of hypokalemia, Na +-containing drugs – edema and increased blood pressure. NSAIDs and ethanol increase the risk of ulceration of the gastrointestinal mucosa and bleeding, Estrogens (including oral estrogen-containing contraceptives) reduce the clearance of ACS, prolong T1 / 2 and their therapeutic and toxic effects. The appearance of hirsutism and acne is facilitated by the simultaneous use of other steroid hormonal drugs – androgens, estrogens, anabolic agents, oral contraceptives. Tricyclic antidepressants can increase the severity of depression caused by taking ACS (not shown for the treatment of these side effects). The risk of developing cataracts increases with the use of other ACS, antipsychotic drugs (neuroleptics), carbutamide and azathioprine. Concurrent administration with m-cholin blockers (including antihistamine drugs, tricyclic antidepressants), nitrates contributes to the development of increased intraocular pressure. prepared on the culture of human diploid cells, as the latter has a high immunogenicity and induces active antiviral immunity.
Immunoglobulin administration may adversely affect the effectiveness of vaccines containing attenuated live measles, rubella, mumps, or chickenpox. Therefore, an interval of 3 months should be observed between the administration of Rebinolin and the attenuated live vaccine.
Compatible with antitubercular serum and antibiotics.
Storage Conditions
At 2 to 8 ° C. Do not freeze. Keep out of reach of children.
Shelf life
2 years.
Deystvuyushtee substance
Immunoglobulin antirabicheskiy
Terms of dispatch from
pharmacies Prescription from
Le
dosage form injection
Possible product names
Rebinolin 150 IU / ml 2ml No. 1 fl