Description
Pharmacological action
Pharmacodynamics
Fluoroquinolone, broad-spectrum antimicrobial bactericidal agent. It blocks DNA gyrase (topoisomerase II) and topoisomerase IV, disrupts supercoiling and cross-linking of DNA breaks, inhibits DNA synthesis, and causes deep morphological changes in the cytoplasm, cell wall and membranes.
Levofloxacin is active against the following strains of microorganisms, both in vitro and in vivo.
Sensitive microorganisms of the IPC:
Aerobic gram-positive microorganisms: Corynebacterium diphtheriae, Enterococcus faecalis, Enterococcus spp., Listeria monocytogenes, Staphylococcus coagulase-negative methi-sensitive (meticillin-sensitive methyl-sensitive, moderate -sensitive strains), Staphylococcus epidermidis methi-S (methicillin-sensitive strains), Staphylococcus spp. (CNs – leukotoxin-containing. Streptococci groups C and G (including Streptococcus agalactiae, Streptococcus pneumoniae peni-S / UR (penicillin-sensitive / moderately sensitive / resistant strains)), Streptococcus pyogenes, Viridans streptococline R-peni -sensitive / resistant strains)
Aerobic gram-negative microorganisms: Acinetobacter baumannil, Acinetobacter spp., Actinobacillus actinomycetemcomitans, Citrobacter freundii, Eikenella corrodens, Enterobacter aerogenme, Enterobacter agglomepperglomerans. vaginalis, Haemophilus ducreyi, Haemophilus influenzae ampi-S / R (ampicillin-sensitive / resistant strains), Haemophilus parainfluenzae, Helicobacter pylori, Klebsiella spp. (including Klebsiella oxytoca, Klebsiella pneumoniae), Moraxela catarrhalis + / – (strains producing and non-producing P-lactamase), Morganella morganii, Neisseria gonorrhoeae non-PPNG / PPNG (strains producing and non-producing penicillinase), Neisseria meningitidis, Pasteurella spp. (including, Pasteurella conis, Pasteurella dagmatis, Pasteurella multocida), Proteus mirabilis, Proteus vulgaris, Providencia spp. (including Providencia rettgeri, Providencia stuartii), Pseudomonas spp. (including Pseudomonas aeruginosa), Serratia spp. (including Salmonella spp., Serratia marcescens).
Anaerobic microorganisms: Bacteroides jragilis, Bifidobacterium spp., Clostridium perfringens, Fusobacterium spp., Peptostreptococcus spp., Propionibacterum spp., Veilonella spp.
Other microorganisms: Bartonella spp., Chlamydia pneumoniae, Chlamydia psittaci, Chlamydia trachomatis, Legionella pneumophila, Legionella spp., Mycobacterium spp. (including Mycobacterium leprae, Mycobacterium tuberculosis, Mycoplasma hominis, Mycoplasma pneumoniae), Ricketsia spp., Ureaplasma urealyticum.
Moderately susceptible microorganisms (BMD> 4 mg / L):
Aerobic gram-positive microorganisms: Corynebacterium urealiticum, Corynebacterium xerosis, Enterococcus faecium, Staphylococcus epidermidis methylic-resistant strains (methicillin-resistant resistant strains, methylicin-resistant strains) .
Aerobic gram-negative microorganisms: Burkholderia cepacia, Campilobacter jejuni, Campilobacter coli.
Anaerobic microorganisms: Bacteroides thetaiotaomicron, Bacteroides vulgatus, Bacteroides ovaius, Prevotella spp., Porphyromonas spp.
Resistant microorganisms (BMD> 8 mg / L):
Aerobic gram-positive microorganisms: Corynebacterium jeikeium, Staphylococcus aureus methi-R (methicillin-resistant strains), Staphylococcus coagulase-negative methi-R (coagulase-negative methicillin-resistant strains).
Aerobic gram-negative microorganisms: Alcaligenes xylosoxidans.
Other microorganisms: Mycobacterium avium.
Pharmacokinetics
When ingested, it is rapidly and almost completely absorbed (food intake has little effect on the speed and completeness of absorption). Bioavailability is 99%.
The time to reach the maximum concentration (Tmax) is 1-2 hours with 250 and 500 mg, the average maximum concentration (Cmax) is 2.8 and 5.2 Ñg / ml, respectively. Communication with plasma proteins – 30-40%.
It penetrates well into organs and tissues: lungs, bronchial mucosa, sputum, genitourinary system, polymorphic nuclear leukocytes, alveolar macrophages. In the liver, a small portion is oxidized and / or deacetylated. It is excreted mainly by the kidneys by glomerular filtration and tubular secretion. The half-life (T ) Is 6-8 hours. Renal clearance is 70% of the total clearance. Less than 5% of levofloxacin is excreted as metabolites.
In urine, over a period of 24 hours, 70% is found unchanged, and over 48 hours – 87% of an oral dose. In feces, over a period of 72 hours, 4% of the oral dose is detected. In renal failure, a decrease in clearance of the drug and its excretion by the kidneys depends on the degree of decrease in creatinine clearance (CC).
Indications
Infectious and inflammatory diseases caused by microorganisms sensitive to levofloxacin:
n – acute pneumonia –
– complicated urinary tract infections (including pyelonephritis)
– infections of the skin and soft tissues (complicated).
Contraindications
– Hypersensitivity to levofloxacin, other quinolones or other components of the drug
– impaired renal function (with CC less than 20 ml / min due to the inability to dose this dosage form)
– epilepsy if we had previously had a lesion
– pseudoparalytic myasthenia gravis (myasthenia gravis)
– children and adolescents under 18 years of age (due to incomplete skeleton growth, since the risk of damage to the cartilaginous growth points cannot be completely excluded)
– pregnancy and the period of breastfeeding (lactation).
Precautions:
– for diseases of the central nervous system (CNS), including those suspicious of CNS involvement, predisposing to seizures and lowering the threshold for convulsive activity of the brain
– in patients who are simultaneously receiving drugs that lower the threshold for convulsive readiness of the brain (cm. section Interaction with other drugs )
– in patients with a history of psychosis and psychiatric illness
– in patients with latent or manifest glucose-6-phosphate dehydrogenase deficiency (increased risk of hemolytic reactions in the treatment of quinolones)
– in patients with impaired function kidneys with QC of 20-50 ml / min (mandatory monitoring of renal function is required, as well as correction of the dosage regimen, see section “Dosage and administration”)
– in patients with known risk factors for lengthening QT shaft: in elderly patients, female patients, patients with uncorrected electrolyte disorders (hypokalemia, hypomagnesemia) with a syndrome of congenital prolongation of the QT interval with heart disease (heart failure, myocardial infarction, bradycardia) while taking medications that can extend the QT interval (see Interaction with other medicines )
– in patients with diabetes mellitus receiving oral hypoglycemic (eg, glibenclamide) or insulin (increased risk of hypoglycemia)
– in patients with severe adverse reactions to other fluoroquinolones, such as severe neurological reactions (increased risk of similar adverse reactions with levofloxacin).
Use during pregnancy and lactation
Levofloxacin is contraindicated for use in pregnant and lactating women.
Specific instructions
Hospital infections caused by Pseudomonas aeruginosa (Pseudomonas aeruginosa) may require combination treatment. The prevalence of acquired resistance of seeded strains of microorganisms may vary by geographic region and over time. In this regard, information on drug resistance in a particular country is required.
For the treatment of severe infections or in case of treatment failure, a microbiological diagnosis should be established with the isolation of the pathogen and determination of its sensitivity to levofloxacin.
Methicillin-resistant Staphylococcus aureus
It is highly likely that methicillin-resistant Staphylococcus aureus will be resistant to fluoroquinolones, including levofloxacin. Therefore, levofloxacin is not recommended for the treatment of established or suspected infections caused by methicillin-resistant Staphylococcus aureus, if laboratory tests have not confirmed the sensitivity of this microorganism to levofloxacin.
Patients prone to seizures
Like other quinolones, levofloxacin should be used with great caution in patients with a tendency to seizures. Such patients include patients with previous lesions of the central nervous system, such as a stroke, severe traumatic brain injury, patients simultaneously receiving drugs that lower the threshold for cerebral seizure, such as fenbufen and other similar non-steroidal anti-inflammatory drugs or other drugs that lower the threshold convulsive readiness, such as theophylline (see section “Interaction with other drugs”).
Pseudomembranous colitis
Developed during or after treatment with levofloxacin, diarrhea, especially severe, persistent and / or blood, may be a symptom of pseudomembranous colitis caused by Clostridium difficile. In case of suspected development of pseudomembranous colitis, treatment with levofloxacin should be stopped immediately and specific antibiotic therapy should be started immediately (vancomycin, teicoplanin or metronidazole by mouth). Drugs that inhibit intestinal motility are contraindicated.
Tendonitis
Rarely observed tendinitis with quinolones, including levofloxacin, can lead to rupture of tendons, including the Achilles tendon. This side effect can develop within 48 hours after the start of treatment and can be bilateral. Elderly patients are more prone to the development of tendonitis. The risk of tendon rupture may increase while taking glucocorticosteroids.
If suspected of tendonitis, discontinue treatment with Levolet ® R immediately and begin appropriate treatment of the affected tendon, for example, providing him with sufficient immobilization (see sections “Contraindications” and “Side effects”).
Hypersensitivity Reactions
Levofloxacin can cause serious, potentially fatal, hypersensitivity reactions (angioedema, anaphylactic shock), even with initial doses (see section ² ÑSide effects ² Ñ). Patients should immediately stop taking the drug and consult a doctor.
Severe bullous reactions
When taking levofloxacin, cases of severe bullous skin reactions, such as Stevens-Johnson syndrome or toxic epidermal necrolysis, have been observed (see section ² ÑSide effects ² Ñ). In case of development of any reactions from the skin or mucous membranes, the patient should immediately consult a doctor and not continue treatment until his consultation.
Hepatic and biliary tract disorders
Cases of hepatic necrosis have been reported, including the development of fatal liver failure with levofloxacin, mainly in patients with severe underlying diseases, such as sepsis (see section ² ÑSide effects ² Ñ). Patients should be warned about the need to discontinue treatment and urgently need to see a doctor in case of signs and symptoms of liver damage, such as anorexia, jaundice, dark urine, itching and abdominal pain.
Patients with renal failure
Since levofloxacin is excreted mainly through the kidneys, patients with impaired renal function require mandatory monitoring of renal function, as well as correction of the dosage regimen (see section “Dosage and Administration”). When treating elderly patients, it should be borne in mind that patients of this group often have impaired renal function (see section “Dosage and Administration”).
Prevention of photosensitization reactions
Although photosensitization is very rare with levofloxacin, patients are not recommended to undergo strong sunlight or artificial ultraviolet radiation (for example, visiting a solarium) without special need during the treatment and for 48 hours after treatment with levofloxacin .
Superinfection
As with other antibiotics, the use of levofloxacin, especially for a long time, can lead to increased reproduction of insensitive microorganisms (bacteria and fungi), which can cause changes in microflora, which is normally present in humans. As a result, superinfection may develop. Therefore, during the course of treatment, it is imperative to re-evaluate the patient’s condition, and, if superinfection develops during treatment, appropriate measures should be taken.
QT prolongation
Very rare cases of QT prolongation have been reported in patients taking fluoroquinolones, including levofloxacin. When using fluoroquinolones, including levofloxacin, caution should be exercised in patients with known risk factors for prolonging the QT interval: in patients with uncorrected electrolyte disturbances (with hypokalemia, hypomagnesemia) with congenital prolongation of the QT interval with heart diseases (heart failure, myocardial infarction, bradycardia) while taking medications that can extend the QT interval, such as class IA and III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics.
Elderly and female patients may be more sensitive to drugs that extend the QT interval.
Therefore, fluoroquinolones, including levofloxacin, should be used with caution (see sections “With caution”, “Dosage and administration”, “Side effects”, “Overdose” and “Interaction with other drugs”).
Patients with glucose-6-phosphate dehydrogenase deficiency
Patients with latent or manifest deficiency of glucose-6-phosphate dehydrogenase have a predisposition to hemolytic reactions when treated with quinolones, what should be taken into account when treating levofloxacin.
Hypo- and hyperglycemia (dysglycemia)
As with other quinolones, when levofloxacin was used, cases of hyperglycemia and hypoglycemia were observed, usually in patients with diabetes mellitus receiving concomitant treatment with oral hypoglycemic drugs (for example, glibenclamide) or insulin preparations. Cases of hypoglycemic coma have been reported. In patients with diabetes mellitus, monitoring of blood glucose concentration is required (see the section “Side effects”).
Peripheral neuropathy
Patients taking fluoroquinolones, including levofloxacin, have sensory and sensory-motor peripheral neuropathy, the onset of which can be quick. If the patient has symptoms of neuropathy, the use of levofloxacin should be discontinued. This minimizes the possible risk of irreversible changes.
Exacerbation of pseudoparalytic myasthenia gravis
Fluoroquinolones, including levofloxacin, are characterized by neuromuscular blocking activity and may increase muscle weakness in patients with pseudoparalytic myasthenia. In the post-marketing period, adverse reactions were observed, including pulmonary insufficiency, requiring mechanical ventilation, and death, which were associated with the use of fluoroquinolones in patients with pseudoparalytic myasthenia. The use of levofloxacin in patients with an established diagnosis of pseudoparalytic myasthenia gravis is not recommended (see section “Side effects”).
Use in an airborne droplet infection with anthrax
The use of levofloxacin in humans according to this indication is based on data on sensitivity to it of Bacillus anthracis obtained in in vitro and experimental studies in animals, as well as on limited data on the use of levofloxacin in person. The attending physician should refer to national and / or international documents that reflect the common point of view on the treatment of anthrax.
Psychotic reactions
When quinolones, including levofloxacin, were used, psychotic reactions were reported that, in very rare cases, progressed to the development of suicidal thoughts and behavioral disorders, causing self harm (sometimes after taking a single dose of levofloxacin (see section “Side effects”)). With the development of such reactions, treatment with levofloxacin should be discontinued and appropriate therapy should be prescribed.
Caution is advised to administer the drug to patients with psychosis or to patients with a history of mental illness.
Visual impairment
If any visual impairment develops, an immediate consultation with an ophthalmologist is necessary (see section ² ÑSide effects ² Ñ).
Effect on laboratory tests
In patients taking levofloxacin, the determination of opiates in the urine can lead to false-positive results, which should be confirmed by more specific methods. Levofloxacin can inhibit the growth of Mycobacterium tuberculosis and subsequently lead to false negative results of a bacteriological diagnosis of tuberculosis. Such side effects of the drug Levolet ® R, like dizziness or vertigo, drowsiness, and visual disturbances (see the section ² ÑSide effects ² Ñ), can reduce psychomotor reactions and the ability to concentrate. This may pose a certain risk in situations where these abilities are of particular importance (for example, when driving, servicing machines and mechanisms, and performing work in an unstable position).
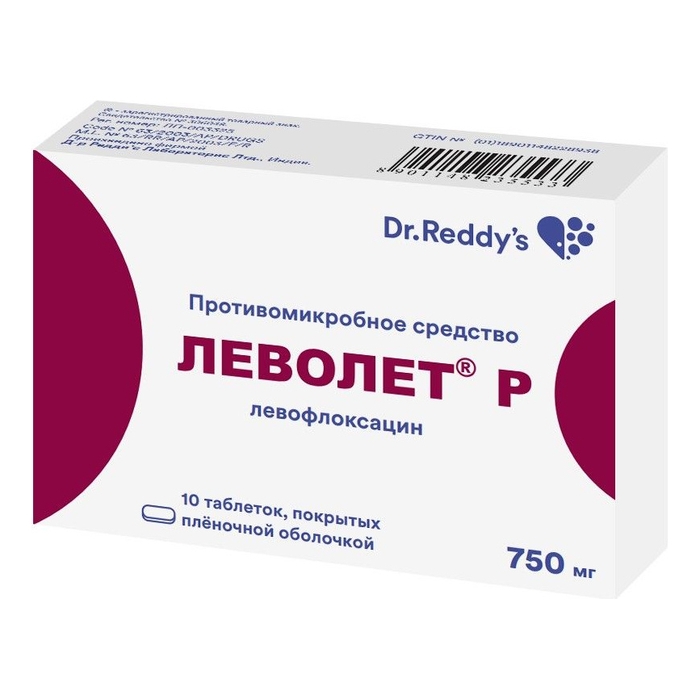
Composition of
Each film-coated tablet 750 mg contains:
Active ingredient:
levofloxacin hemihydrate 768.7 mg, equivalent to 750 mg of levofloxacin.
Excipients:
microcrystalline cellulose (Avicel PH 101) 76 mg,
corn starch 75.3 mg,
silicon dioxide colloidal 15 mg,
crospovidone 64 mg,
hypromellose (15 cps) microcrystalline avr cellulose (15 cps 102) 90 mg
magnesium stearate 15 mg
Film coat:
opadray white OY 58900 (hypromellose 5 cP 62.5%, titanium dioxide (E171) 31.25%, macrogol-400 6.25%) 28 mg.
Dosage and administration
The drug Levolet ® R is taken orally once a day. Tablets should be taken without chewing and drinking plenty of fluids (from 0.5 to 1 cup). The drug can be taken before meals or at any time between meals.
The drug should be taken at least 2 hours before or 2 hours after taking antacids containing magnesium and / or aluminum, salts of iron or sucralfate (see section ² ÑInteraction with other medicines ² Ñ).
Doses are determined by the nature and severity of the infection, as well as the sensitivity of the suspected pathogen. Do not exceed recommended dose.
The duration of treatment varies depending on the course of the disease. Given that the bioavailability of levofloxacin when taken in tablets is 99%, in the case of a patient transferring from an intravenous infusion of Levolet ® R to taking Levolet ® R tablets, treatment should be continued in the same dose that was used for intravenous infusion. The recommended dosage regimen and duration of treatment in patients with normal or mildly reduced renal function (CC more than 50 ml / min).
Acute bacterial sinusitis: 750 mg once a day, 5 days of treatment.
Community-acquired pneumonia, caused by Streptococcus pneumoniae (penicillin-sensitive / moderately sensitive / -resistant), Haemophilus influenzae (ampicillin-sensitive / -resistant), Haemophilus parainfluenzae, Mycoplasma pneumonia, Chlamydia pneumoniae: 750 mg 1 time per day, course of treatment 5 times a day.
Complicated urinary tract infections caused by Escherichia coli, Klebsiela pneumoniae, Proteus mirabilis acute pyelonephritis caused by Escherichia coli, including cases of absent bacteremia: 750 mg once a day, 5 days of treatment.
Complicated infections of the skin and soft tissues: 750 mg 1 time per day, course of treatment 7-14 days.
Dosing regimen in patients with impaired renal function (CC 50 – 20 ml / min).
Levofloxacin is excreted mainly through the kidneys, therefore, in the treatment of patients with impaired renal function (CC 50 – 20 ml / min), a dose reduction is required: the recommended dose is 750 mg every 48 hours.
Dosage regimen in patients with impaired liver function
In case of impaired liver function, dosage adjustment is not required, since levofloxacin is metabolized in the liver to a very small extent.
Dosing regimen in elderly patients
For elderly patients, no dosage regimen correction is required, except for cases when creatinine clearance is reduced to 50 ml / min or lower.
Side effects
The following side effects are presented in accordance with the following gradations of their frequency of occurrence: very often (? 1/10) often (? 1/100, <1/10) infrequently (? 1/1000, <1/100) rarely (? 1/10000, <1/1000) very rarely (<1/10000) (including individual messages) the frequency is unknown (according to the available data, it is not possible to determine the frequency of occurrence). Data obtained in clinical trials and in the post-marketing use of the drug Disorders of the heart Rarely: sinus tachycardia, palpitations. Frequency unknown (post-marketing data): QT interval lengthening, ventricular arrhythmias, ventricular tachycardia, ventricular tachycardia of the pirouette type, which can lead to cardiac arrest (see sections Overdose, Special instructions). Disorders of the blood and lymphatic system Infrequently: leukopenia (a decrease in the number of white blood cells in the peripheral blood), eosinophilia (increase in the number of eosinophils in the peripheral blood). Rarely: neutropenia (a decrease in the number of neutrophils in the peripheral blood), thrombocytopenia (a decrease in the number of platelets in the peripheral blood). Frequency unknown (post-marketing data): pancytopenia (decrease in the number of all shaped elements in peripheral blood), agranulocytosis (absence or sharp decrease in the number of granulocytes in peripheral blood), hemolytic anemia. Disorders of the nervous system Often: headache, dizziness. Infrequently: drowsiness, tremor, dysgeusia (perversion of taste). Rarely: paresthesia, convulsions (see section “Special instructions”). Frequency unknown (post-marketing data): peripheral sensory neuropathy, peripheral sensory-motor neuropathy (see section Special Instructions), dyskinesia, extrapyramidal disorders, ageusia (loss of taste), parosmia (disorder of sensation of smell, especially subjective sensation of smell, objectively absent), including loss of smell, fainting, benign intracranial hypertension. Visual impairment Rarely: visual impairment, such as blurry images. Frequency unknown (post-marketing data): transient loss of vision, uveitis. Hearing impairment and labyrinthine disorders Infrequently: vertigo (feeling of rejection or spinning or of one’s own body or surrounding objects). Rarely: tinnitus. Frequency unknown (post-marketing data): hearing loss, hearing loss. Disorders of the respiratory system, chest and mediastinal organs Uncommon: shortness of breath. Frequency unknown (post-marketing data): bronchospasm, allergic pneumonitis. Disorders of the gastrointestinal tract Often: diarrhea, vomiting, nausea. Infrequently: abdominal pain, dyspepsia, flatulence, constipation. Frequency unknown (post-marketing data): hemorrhagic diarrhea, which in very rare cases can be a sign of enterocolitis, including pseudomembranous colitis (see section “Special instructions”), pancreatitis. Disorders of the night and urinary tract Infrequently: increased serum creatinine concentration. Rarely: acute renal failure (for example, due to the development of interstitial nephritis). Disorders of the skin and subcutaneous tissue Infrequently: rash, itching, urticaria, hyperhidrosis. Frequency unknown (post-marketing data): toxic epidermal necrolysis, Stevens-Johnson syndrome, exudative erythema multiforme, photosensitivity reactions (hypersensitivity to solar and ultraviolet radiation) (see section “Special instructions”), leukocytoclastic vasculitis, stomatitis. Reactions from the skin and mucous membranes can sometimes develop even after taking the first dose of the drug. Disorders of the musculoskeletal system and connective tissue Infrequently: arthralgia, myalgia. Rarely: tendon damage, including tendonitis (eg, Achilles tendon), muscle weakness, which can be especially dangerous in patients with pseudoparalytic myasthenia gravis (see myasthenia gravis). Frequency unknown (post-marketing data): rhabdomyolysis, tendon rupture (e.g., Achilles tendon). This side effect can be observed within 48 hours after the start of treatment and can be bilateral in nature (see also the section Special Instructions), rupture of ligaments, rupture of muscles, arthritis. Metabolism and nutritional disorders Infrequently: anorexia. Rarely: hypoglycemia, especially in patients with diabetes mellitus (possible signs of hypoglycemia: wolf appetite, nervousness, perspiration, trembling). Frequency unknown: hyperglycemia, hypoglycemic coma (see section “Special instructions”). Infectious and parasitic diseases Infrequently: fungal infections, development of resistance of pathogenic microorganisms. Vascular disorders Rarely: lowering blood pressure. Common disorders Infrequently: asthenia. Rarely: pyrexia (fever). Frequency unknown: pain (including back, chest, and limb pain). Immune system disorders Rarely: angioedema. Frequency unknown (post-marketing data): anaphylactic shock, anaphylactoid shock. Anaphylactic and anaphylactoid reactions can sometimes develop even after taking the first dose of the drug. Disorders from the liver and biliary tract Often: increased activity of liver enzymes in the blood (for example, alanine aminotransferase (ALT), aspartate aminotransferase (ACT), increased activity of alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT). Infrequently: increased concentration of bilirubin in the blood. Frequency unknown (post-marketing data): severe liver failure, including cases of acute liver failure, sometimes fatal, especially in patients with a serious underlying disease (for example, patients with sepsis) (see Special Instructions) hepatitis, jaundice. Mental disorders Often: insomnia. Infrequently: a feeling of anxiety, anxiety, confusion. Rarely: mental disorders (eg, hallucinations, paranoia), depression, agitation (agitation), sleep disturbances, nightmares. Frequency unknown (post-marketing data): mental disorders with behavioral disorders causing self-harm, including suicidal thoughts and suicidal attempts. Other possible unwanted effects related to all fluoroquinolones Very rare: attacks of porphyria (a very rare metabolic disease) in patients with porphyria. Storage conditions At a temperature not exceeding 25C. Keep out of the reach of children! Shelf life 3 years. active substance Levofloxacin Terms and conditions prescription Dosage form tablet Appointment Adults doctor’s prescription